Plantar Fasciitis / Heel Spurs
Plantar Fasciitis & Heel Spurs
Plantar Fasciitis & Heel Spurs
DEFINITION:
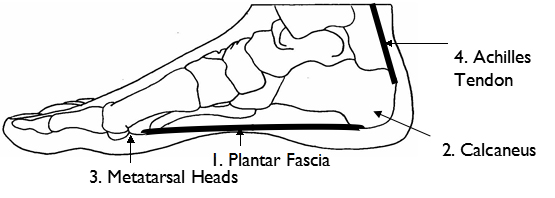
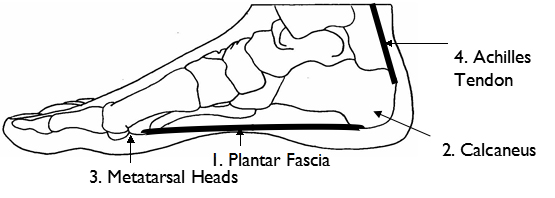
The plantar fascia1 is a tough fibrous ligament on the sole of the foot. It extends from the calcaneum2 (heel) to the metatarsal heads3 (toes) and acts to maintain the arch of the foot. Plantar fasciitis is the term used to describe inflammation of the plantar fascia1.
SYMPTOMS:
Pain at the origin of the plantar fascia1 at the calcaneum2, particularly when:
The area is markedly tender and often also slightly swollen.
A spur at the calcanuem2 (a bony growth on the heel).
CAUSES:
Whenever weight is put through the foot, the plantar fascia1 is under tension and stretched. Repeated stretch of the fascia fatigues it. The natural repair mechanism cannot keep up with the fatigue. This can be due to:
strain on the arch and subsequent inflammation of the plantar fascia1)
SURGERY:
In extreme cases a surgical release (excision of the inflamed tissue and a release of nerves in the heel) is the last option available. Rarely will a heel spur be excised, non-surgical options should be exhausted first.
TREATMENT:
Don’t wait for it to get better – there are many things which can be done!
Treatment should be initially aimed at decreasing the inflammation, keeping the fascia at its natural length (to decrease fiber disruption) and to cushioning.
Ice Program:
Place a can of drink, straight from the fridge, onto the floor. Place your foot on top of the can so the curved surface of the can sits in the arch of your foot. Roll your foot back and forth over the can. This will gently stretch your plantar fascia to its natural length, create an arch in your foot and decrease the inflammation of the plantar fascia due to the very cold can.
Frequency: 10 minutes morning and night
Stretching Program:
 Place your hands on the Sit with your legs Wall and have your feet straight in front of you pointing forward. keep place a belt or towel your back leg straight around your foorand and heel on the ground, You then bend your front knee should feel the stretch forward.You should feel toward the bottom of the stretch all the way muscle & down your calf muscle.tendon.
Place your hands on the Sit with your legs Wall and have your feet straight in front of you pointing forward. keep place a belt or towel your back leg straight around your foorand and heel on the ground, You then bend your front knee should feel the stretch forward.You should feel toward the bottom of the stretch all the way muscle & down your calf muscle.tendon. Place your hands on the wall your feet close together, as well as close to the wall, pointing fwd. keeping both heels on the ground, bend both knees fwd. You should feel the stretch toward the bottom of your calf muscle & Achilles tendon.
Place your hands on the wall your feet close together, as well as close to the wall, pointing fwd. keeping both heels on the ground, bend both knees fwd. You should feel the stretch toward the bottom of your calf muscle & Achilles tendon. Place your hands on the wall. Place one foot up against the wall and keep the leg straight. Lean forward toward the wall You should feel the stretch all the way down your calf muscle. Your calf Achilles
Place your hands on the wall. Place one foot up against the wall and keep the leg straight. Lean forward toward the wall You should feel the stretch all the way down your calf muscle. Your calf Achilles Place Your calf Achilles
Place Your calf AchillesFrequency: 30 seconds each side, four times a day
Assessment & Correction of Underlying Biomechanical Causes: of Plantar Fasciitis:
Consult your Orthopaedics Australia Orthotist for an opinion. A full examination of your feet including palpation, gait analysis, lifestyle and footwear analysis will be completed to ensure accurate diagnosis. Orthotics are the best treatment modality for this particular condition. A thick heel pad is a good start in determining whether an Orthotic will be needed. If the pain is relieved with a heel pad, an Orthotic will offer a better permanent solution. Orthotics distribute the weight of your body to other areas of the foot, unloading the heel as well as cushioning the painful area. Careful consideration should also be given to footwear (supportive shoes with a soft sole are the best type of footwear for this condition).