Soft tissue injuries can broadly be divided into two types – acute and overuse (or chronic). Acute soft tissue injuries involve muscles, tendons and ligaments, and occur in an instant causing sudden pain, disability and swelling. Examples are ankle sprains and torn muscles. Overuse soft tissue injuries, on the other hand, are characterised by a gradual increase in pain and disability and are caused by a gradual overload on tendons and ligaments. Examples are tendonitis, ‘shin splints’ and tennis elbow. Exercises and medication prescribed by your doctor are essential for treating soft tissue injuries. The following guide will set your mind at ease so keep it close by for handy reference.
Acute injuries
The three types of acute soft tissue injuries are:
- Contusions – bleeding into a tissue as a result of a direct blow
- Strains – tearing of a muscle or tendon
- Sprains – tearing of a ligament or joint capsule
The first Step – RICE
The following measures should be taken immediately and for the next 72hours following an acute injury.
Rest: Stop using the injured site and rest your body generally.
Ice: Apply crushed ice in a moist cloth to the injured site for 15 to 20 minutes and repeat every one to two hours.
Compression: After the ice application, apply a firm rubberised bandage.
Elevation: If possible, keep the injured part above the level of your heart.
Management
Your GP will give advice that will cover the following areas:
Rest
If there is a tissue weakness the injury should be rested completely. This can be done by putting a splint on the injury which will limit your normal activities. Pain is usually a good indicator of whether you are exercising too much. Remember, while rest is important some exercises will speed your recovery.
Medication
You may need anti-inflammatory medication for a few days to provide some pain relief and to treat the tissue inflammation. Your GP will discuss your medication with you.
Exercise
This will involve stretching and strengthening the injured site and your body in general. Look below for some recommendations, although your GP may give you more specific exercises as well.
Overuse injuries
These chronic injuries (which develop slowly) can usually be divided into groups:
- Overloading a muscle, or more commonly, a tendon (tendonitis)
- Sprains to ligaments or joint capsules
Causes
Overuse injuries are caused by doing too much of one activity – this may be too often, too hard or for too long. They can also be caused by doing the activity incorrectly. People vary in their ability to cope with repetitious activity and an overuse injury may represent an inbuilt ‘weakness’ placing that person at risk of repeated injury. An example is flat feet causing excessive foot twisting (or pronation) resulting in Achilles tendonitis or shin splints.
Management
Your GP will give you specific advice that may include:
Rest
Stopping the activity causing the excessive loading of your tissues is vital.
Anti-Inflammatory treatment
This may involve medication (taken by mouth or applied to the skin), applying ice or heat to the injury, or physiotherapy.
Exercise
As there is a tissue weakness, stretching and strengthening exercises will be essential for a complete recovery. Examples and guidelines for these are below but your GP will probably give you more specific ones.
Correcting an underlying cause
This may require a referral to another doctor, podiatrist (as in the case of flat feet), or professional to have your technique analysed. Ask your GP if this is necessary.
stretching exercises
These exercises should involve the site of the injury as well as your entire body. They restore length and some strength to the injured tissue and maintain full function of non-injured parts. Stretching exercises should be done slowly, without pain and without bouncing. Try to hold these stretches for about 5-10 seconds and do 5 sets of them 2 or 3 times a day.

Front Thigh –
Hold on to a wall for support. With knees together, pick up leg and hold the foot towards the buttocks; pull back gently. Repeat on other side.
Calf Stretch –
Place heels on the ground and the balls of the feet on a book, with the legs straight.
Other specific exercises will vary according to the injured site and will be given to you by your GP or physiotherapist.
strengthening exercises
These exercises involve a progressive increase in the resistance you apply and the number of times they are performed (repetitions). These exercises should be done gradually, regularly and usually under supervision. They are designed to strengthen the weakened tissue and maintain your general body strength. Try to do them in 3 or 4 sets of 10-30 repetitions every day.

Calf –Rise up onto toes, hold for 2 seconds then down. With time, add speed, weight, and then use each leg separately.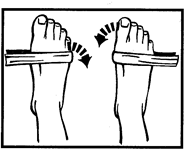
Ankle –Loop a piece of rubber over the foot and with a fixed heel, do exercises inwards and outwards.
returning to activity
Becoming active again will depend on your injury, so make sure you follow your doctor’s instructions. Generally, this will involve a progressive and gradual to physical activity, sport and work.
In the case of a lower limb injury, start with walking as early as possible, swimming, cycling and then jogging if appropriate. Do this 3 or 4 times a week for 25 to 40 minutes.
With any injury, it’s vital to maintain some level of fitness throughout your recovery with an exercise such as walking. Allow about 15 minutes to warm up and stretch. Following exercise, allow 5 minutes to cool down and stretch. Remember to slow down or stop if you are experiencing pain
Exercise tip: Before any strenuous exercise, allow 15 minutes to warm up and stretch muscles. This will help prevent further injuries.
