 What is it?
What is it?
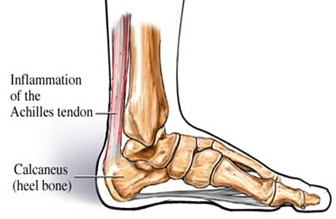
Achilles tendonitis is a painful and often debilitating inflammation of the Achilles tendon (heel cord). The Achilles tendon is the largest and strongest tendon in the body. It is located in the back of the lower leg, attaches to the heel bone (calcaneus), and connects the leg muscles to the foot. The Achilles tendon gives us the ability to rise up on our toes, facilitating the act of walking, and Achilles tendonitis can make walking almost impossible.
Symptoms
In most cases symptoms develop gradually. Pain may be mild at first and worsen with continued activity. Repeated or continued stress on the Achilles tendon increases inflammation and may cause it to rupture. Partial or complete rupture results in traumatic damage and severe pain, making walking virtually impossible and requiring a long recovery period. Patients with tendonitis may experience a sensation of fullness in the back of the lower leg or develop a hard knot of tissue (nodule).
Causes
Overuse; Too much too soon is the basic cause of overuse injuries, however other factors can make an overuse injury more likely.
Running up hills will mean the Achilles tendon has to stretch more than normal on every stride. This is fine for a while but will mean the tendon will fatigue sooner than normal.
Over-pronation or feet which roll in can place an increased strain on the Achilles tendon. As the foot rolls in (flattens) the lower leg rotates inwards also which twists the Achilles tendon place twisting stresses as well as stresses along its length.
Wearing high heels consistently and then expecting to run 5 miles in flat running shoes puts abnormal strain on the Achilles tendon making it stretch further than it is comfortable.
Overweight and obesity; being overweight places more strain on many part of the body, including the Achilles tendon.
Treatment
Treatment for Achilles tendonitis depends on the severity of the injury. If heel pain, tenderness, swelling, or discomfort in the back of the lower leg occurs, physical activity that produces the symptoms should be discontinued.
If the problem returns or persists, a medical professional should be consulted. If pain develops even with proper stretching and training techniques, the patient should consult a podiatrist to check for hyper-pronation and adequate arch support. The addition of an orthotic may be enough to maintain good arch and foot alignment and eliminate pain.
If damage to the tendon is minor, the injury may respond to a simple course of treatment known as RICE (rest, ice, compression, elevation).
Rest the tendon by keeping off their feet as much as possible;
Apply ice packs for 20 minutes at a time every hour for a day or two to reduce swelling;
Compress the ankle and foot with a firmly (not tightly) wrapped elastic bandage; and
Elevate the foot whenever possible to minimize swelling.
A non-steroidal anti-inflammatory drug (NSAID) such as ibuprofen may be used to reduce pain, swelling, and inflammation.
Other treatment that may be recommended:
Placing the foot in a cast or restrictive ankle-boot to minimise movement and give the tendon time to heal. This may be recommended in severe cases and used for about eight weeks.
You may also be given specific exercises to gently stretch the calf muscles once the acute stage of inflammation has settled down. Your doctor, physiotherapist or podiatrist will recommend these exercises when you are on the road to recovery. Recovery is often slow and will depend on the severity of the condition and how carefully you follow the treatment and care instructions you are given.
Surgery is considered the last resort. It is only recommended if all other treatment options have failed after at least six months. In this situation, badly damaged portions of the tendon may be removed. If the tendon has ruptured, surgery is necessary to re-attach the tendon.